What is a registrar? – A ‘who's who’ of public hospital doctors
What, exactly, is a medical registrar? As a medical student, I was told ‘a registrar is a doctor in a training program’. A survey of Google search results shows this view is widespread:
A medical registrar is a doctor who undergoes advanced training in a specific specialty … —Australian Medical Placements
First of all, registrars are medical officers who have enrolled in a specialty training program. —AdvanceMed
Medical registrars are doctors who have completed their medical degree and are undertaking further training in a particular area of medicine. —Healthie
A Registrar is a doctor training to be a Specialist. —St Vincent's Hospital Sydney
In Australia, registrar refers to a senior doctor who has chosen a specialty and is training towards that specialty. —HealthStaff Recruitment
These definitions are incorrect! Let's define what a registrar is – and the other roles in the medical hierarchy of Australian public hospitals.
What's wrong with these definitions?
Defining a registrar as having something to do with specialty training is fundamentally incorrect, because in the average hospital there will be many registrars who are not in training (e.g. unaccredited surgical registrars), and many doctors who are in training but who are not registrars (e.g. basic physician trainees at the resident level).
Fundamentally, ‘registrar’ is an employment classification, which is a separate matter to training progression – though there may be some correlation.
Distinguishing the different domains
It is relevant to consider the domains separately of medical registration, employment classification and specialty training.
Medical registration provides the legal framework for regulating the practice of medicine in Australia, and is administered by Ahpra in accordance with the Health Practitioner Regulation National Law. A newly graduated doctor will practice with provisional registration, meaning they must practice under supervision as an intern. Upon completing internship and gaining general registration, a doctor can practice unsupervised within their own scope of practice. However, to claim some Medicare rebates requires specialist registration, which requires completion of specialty training among other things.1
Employment classification describes the job title of the doctor, which for most hospital doctors will be assigned by the hospital. Registrar is one such level of classification. The employment classification describes the doctor's seniority and responsibilities within the unit, and determines the doctor's rate of pay, though these may vary from unit to unit.
Specialty training is administered by an accredited specialist medical college. Common specialty training programs include general practice, internal medicine (physician training), surgery, emergency medicine, intensive care, anaesthetics, radiology, pathology, and so on.
The following diagram shows the different domains in parallel:
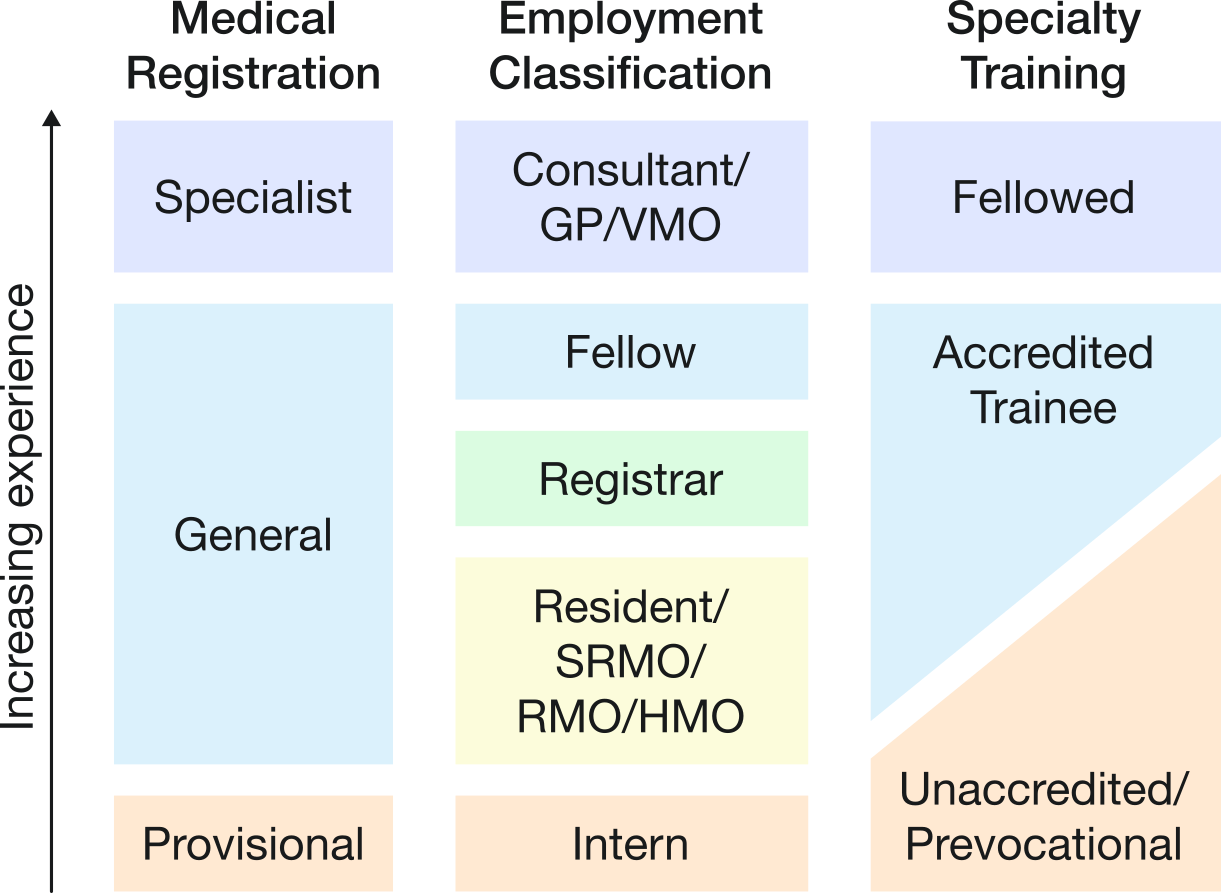
Because one generally progresses through each domain with experience, there is usually some correlation between the domains. For example, an intern will usually have provisional registration, and a consultant will usually have specialist registration. However, because each domain is independent, there may be exceptions – for example, some registrars and fellows may have specialist registration, because they are undertaking further post-fellowship training or are waiting for a consultant position to become available.
Employment classifications – what is a registrar?
A registrar is the junior doctor who manages the day-to-day operation of the unit. A registrar performs all required medical functions, under the supervision of a consultant. For example, a registrar on the ward or in clinic will review patients and make plans. A registrar holding the referrals/consults phone will take calls and see patients or provide advice as required. A surgical registrar in theatre will perform surgeries (within their competence). A radiology registrar will protocol and report studies. A medical registrar on ward cover (e.g. perioperative or after-hours registrar) will review and manage sick patients, and escalate to the home team if required.
Because a registrar is a junior doctor and not fully qualified in that field, a registrar will be supervised by a consultant. The degree of supervision will depend on the unit, and on the competence of the registrar. An experienced surgical registrar who is close to becoming a consultant themselves might personally perform all but the most complex surgeries with only indirect supervision. A very junior surgical registrar may be directly supervised at first even for simple procedures, and is likely to be the assistant rather than primary operator in a more complex procedure.
A consultant, then, is a fully qualified specialist who has ultimate responsibility for the management of patients on their unit. If all the junior doctors are unavailable (say, due to industrial action or illness), the consultant will need to perform all their roles. In practice, a public hospital consultant has a principally supervisory role to the registrars, and their time otherwise will be divided between other high-level leadership functions (e.g. clinical governance, research, teaching).
A fellow (if the unit has one) is a doctor of intermediate grade between a registrar and consultant. The role of a fellow is highly variable between units, and confusingly is unrelated to the concept being a ‘fellow’ of a specialist college. In surgery, a fellow has usually already obtained their specialist qualifications (e.g. general surgery training) and is gaining further training in a subspecialty (e.g. hepatobiliary surgery). In medicine, a fellow usually has not obtained specialist qualifications, and might be regarded as synonymous with a senior registrar.
Junior to registrars are interns and residents. An intern is a doctor in the first year of practice after graduating medical school. A large portion of an intern's duties will be administrative duties such as taking notes on ward rounds, organising investigations, performing procedures such as cannulation and catheterisation, and writing discharge summaries and prescriptions. Particularly after hours, an intern will also review and manage patients who become unwell on the ward and require a medical review.
A resident is of intermediate grade between an intern and registrar. On medical units, residents may have a similar role to the interns focusing on administrative duties and ward work. On surgical units, residents (particularly those with an interest in the field) may develop junior registrar skills such as minor surgical procedures. An equivalent term is resident medical officer (RMO)/senior resident medical officer (SRMO). In Victoria, the more common term is hospital medical officer (HMO), and in Queensland, junior/senior house officer (JHO/SHO).
How does this relate to training?
As mentioned, it is best to think about specialty training as separate to employment. Conceptually, one applies to enter specialty training, which is administered by the college. Separately, one applies for a job at an appropriate classification, which is administered by the hospital. One ensures throughout the process that the job is meeting the specialty training requirements for progression. GP training, emergency medicine training, and advanced physician training are good illustrations of this distinction – where there is a clear separation between applying for training, and applying for jobs.
In many specialities, however, the process is at least somewhat streamlined, which can blur the distinction:
-
In surgery, one applies to the college to enter training. If successful, the college allocates registrar positions to trainees for the duration of training, so there is no separate application for jobs. One enters specialty training as a registrar.
-
In basic physician training, the reverse is true – one applies to the hospital (or training network) for a resident position accredited for basic training. If successful, applying to enter training with the college is essentially a formality. One typically enters specialty training as a resident.
Even in these streamlined cases, however, it is worth keeping in mind the distinction between training and employment, since the college will be responsible for training (e.g. term requirements, educational supervisors, sign-offs), while the hospital will be responsible for employment (e.g. rostering, pay, leave).
A person on a training program is commonly said to be ‘accredited’,2 as opposed to a person not on a training program who is said to be ‘unaccredited’ (or the newfangled ‘prevocational’). A surgical registrar, then, might be an ‘accredited registrar’ or an ‘unaccredited registrar’ (in Queensland also called a principal house officer (PHO)).3
Footnotes
-
The National Law otherwise does not restrict the scope of a general registrant's practice. A PGY2 general registrant could, in theory, perform major surgery unsupervised and there is nothing ‘specific’ in the National Law that would prohibit this. Of course, it would be extremely unlikely that a PGY2 doctor would have the appropriate skills and competence to do so, and so this would be negligent and therefore grounds for disciplinary action under the National Law. ↩
-
A stickler for correctness would argue that the colleges ‘accredit’ hospitals (basic physician training) or training positions (surgery), and not people – but the terminology has stuck. ↩
-
Medical registrars are usually accredited (since entry into training is usually as a resident), but in paediatrics there is the unusual situation where resident positions outnumber training places, hence there are ‘accredited residents’ and ‘unaccredited residents’. I am unaware of any other field where residents are so distinguished. ↩